mccoy
#21
@tj_long
I’ve read the article and it sure shows some evidence of an anomalous alteration of transaminases (except ALP) after weightlifting in people who were not usually training with weights. This is perhaps to construe as deriving from muscular inflammation after a higher-than-usual level of activity.
Going back with memory to my own case, as far as I remember, the baseline, with no alteration of transaminases was measured in similar training conditions as the most recent measurements (a moderate weightlifting routine). It may also be that I worked out intensively 2-4 days before the measurements, but it’s rare since I must restrain myself due to tendon aches. Bottom line, this is something to evaluate attentively.
Presently I tend to assign a significant probability that the elevation in liver enzymes and CK is due mainly to the statin+ezetimibe combo, even if in very low dosages.
My strategy is:
a) leave rosuvastatin away and keep ezetimibe minidose, 2.5 mg/d
b) leave berberine away.
c) decrease saturated fats and foods high in cholesterol. No more egg yolks. Only lowfat cheese in moderate amounts. I’m already eating plenty of fibers.
d) measure lipid panels and enzymes again within 3 months.
1 Like
A_User
#22
You aren’t doing that much and non-HDL already around 110 mg/dl then under this period, what are you measuring for?
100 or 110 mg/dl or even your now result at 90 mg/dl of Non-HDL-c isn’t something to be happy about IMO.
I would target much lower and a mini dose of ezetimibe isn’t going to do anything – pointless to measure. Since we have RCT’s we should know about how much LDL will lower, and you had already previous results.
40 mg/dl non-HDL-c ok… I would target 30 mg/dl (or apoB), at least below 70 mg/dl.
mccoy
#23
AnUser, although you like the 1st percentile, no higher, my present value of Non-HDL = 10th percentile would be all right to me, at least for some time, since I have no other risk factors so far. I might develop some higher fast blood glucose though and I will probably end up with a higher Non-HDL percentile.
I know you are seeing this as an exercise in futility, but an optimization scheme means that a significant reduction in lipid markers cannot be obtained at the expense of a significant increase in liver health markers. Peter Attia confirms that he ceases statin+ezetimibe if that results in a transaminases elevation.
So, since my present tools are only ezetimibe and lifestyle, I’m going to try them and see what percentile I can reach. This is while deciding if to wait for obicetrapib (if not too expensive and assuming it works in my system) or to adopt bempedoic acid (assuming I can spend that money). PCSK9-i’s are out for now.
I’m in no hurry, as we know such strategies are efficacious in the very long term.
A funny note to end up. If I decide to take bempedoic acid, the cost will be double, since my wife will not tolerate that I take it and she doesn’t. Pharmaceuticals from India will be almost inevitably seized at customs.
2 Likes
A_User
#24
Your non-HDL-c without any intervention is 122 mg/dl which is around the 44th percentile (1). Even if Ezetimibe 2.5 mg decreased that by 10% you would be at 110 mg/dl which is above the 25th percentile – higher than Thomas Dayspring would recommend. I would look into some other ways of lowering in that case and research it more. Obicetrapib might be expensive. Lowering non-HDL-c is about the best longevity therapy available, so don’t dismiss the value you will get from researching this, I think.
(1) https://www.sciencedirect.com/science/article/pii/S0735109713030751#tbl1fnlowast
I would personally just quit everything and see liver enzymes decrease first in a relatively new re-test, then add in a therapy like 10 mg ezetimibe and carefully monitor it again.
1 Like
amuser
#25
I think you’re shortchanging yourself if you don’t see what a standalone 10mg ezetimibe can do.
It dropped my ApoB from 90 to 53. By itself. Sustained across multiple weeks.
And my last ALT, AST, and ALP values are the lowest I’ve recorded, of twenty tests in the last two years. At least for me, these numbers vary within a relatively large range. I expect my next to show higher values
2 Likes
mccoy
#26
@A_User, I read the article you posted, it’s fascinating to see the bivariate function of NHDL %-tile versus LDL %-tile within the single triglyceride ranges. It is a linear function with trigs in the range of 100-149 mg/dL and I suspect that for the users of this forum the first left-hand graph is the one to use if curious about percentiles.
Do not let’s forget the reduction hopefully provided by dietary intervention, I hope to add another estimated -10% to my baseline, meaning -20% in total, which would take the %-tile down to the 20th, which may be acceptable in individuals without other risk factors, a subgroup where I’m placed right now.
We agree on that, but the effect seems to be cumulative, so we are probably reaping the benefits in a 10-30 years period. I’m all right with that, since my plan is to hit the 100s with full autonomy. The former means that I have plenty of time to try and find the best strategy.
That sounds sensible, although I can gain some time and testing since I already know my baseline. If the anzimatic baseline is going to be all right with a minidose of ezetimibe, then I know I can increase the minidose gradually, otherwise I’ll have to eliminate all things as you suggest and try other compounds.
tj_long
#27
Yes, but is the elevation coming from the liver or the muscles? As I understand it, statins can also release enzymes from muscles. I couldn’t find a good article at the moment, which I recall was written by a very experienced hepatologist. The main point was that statin-induced ALT elevation is almost never harmful unless it is many times above the reference range.
mccoy
#28
It’s clear, but we should need some preponderance of evidence on this. In the doubt, what MDs do (included the GP who’s following my wife, including Peter Attia) is to exclude the drug(s) under suspicion.
A_User
#29
I’m not sure about that. If anything, the largest effect might be had right now and you don’t get a better time if you can do it safely. Besides, you probably have had a period of cumulative exposure, and if your non-HDL-c has been around the 50th percentile that you wouldn’t have had any protection.
If it’s cumulative and exponential the gains are greatest the earlier you start. I don’t know what you can do if your liver enzymes increase from rosuvastatin. Could other statins work? Is it only in combination with ezetimibe? etc
2 Likes
mccoy
#30
Interesting data on your system. Now, what I’m going to do is to study the response in my own system. Actually, if the minidose turns out to be all right, I think I’ll increase gradually the dosage.
Do not let’s forget that the response constitutes a random variable, with sometime a high degree of variability within a particular group, even though homogeneous.
Some graphs have been posted in this forum, the response is always a random variable, the average is only a reference.
1 Like
mccoy
#31
At this point, the subjective cardiologic tests must be applied, let’s say there is no evidence of anomalous plaque accumulation, but this from indirect inference (carotid intima media, HR stress test). Also, the above non-HDL at the 50th percentile has been the highest that I remember, probably not representative of the lifetime AUC.
There are many variables involved, so the game is going to be an interesting one!
A_User
#32
Once CAC turns positive, that’s already advanced developed disease. It shouldn’t change prevention strategy either way, that’s just for people who are hesitant and doesn’t have the knowledge.
4 Likes
mccoy
#33
All the above of course excluding the possibility of the benefit of plaque regression. There have been so many discussions though, I don’t remember any preponderance of evidence of (significant) regression. My memory may be wrong though.
A_User
#34
Early lesions:
But regression while secondary prevention at max for example 50% blockage to 48% blockage.
1 Like
mccoy
#35
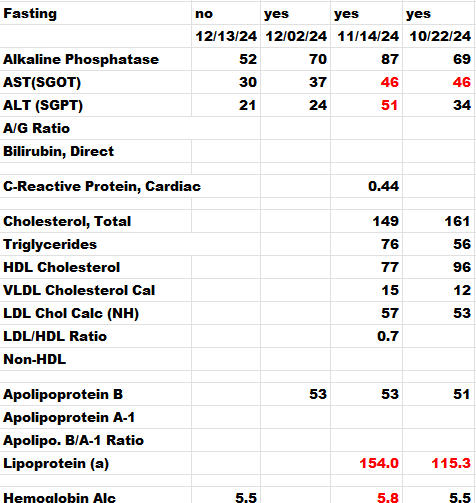
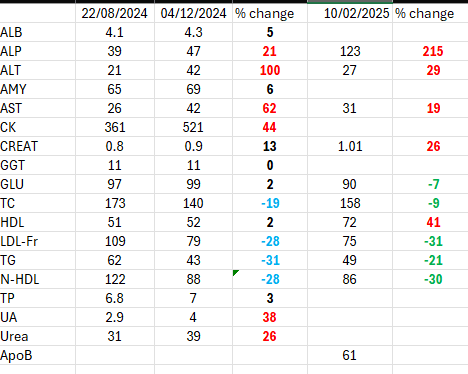
I have an update on the experiment. I dropped the statin and saved the ezetimibe, 2.5 mg/d (one half pill every other day). Plus dietary intervention. Drastically decreased fat cheese, fat yogurt, all but eliminated eggs. I’m eating high fat but mainly plant-derived and no palm oils.
This time I did a venous blood draw, whereas previously it was capillary blood.
The results would suggest that dietary plus minidoses of ezetimibe are about the same as crestor+ezetimibe minidoses at higher amount of dietary saturated fats.
Changes all refer to the baseline. There is the ALP outlier but it may be some transient or even a measurement error.
I think presently I’m going to be satisfied with this, liver enzymes almost back to baseline and ApoB= 10th percentile, non-HDL = 9th percentile. It could be better but I have no other concomitant risk factors like hypertension, adiposity, inflammation. Taking my time to reason about this strategy and seeing what my values are going to be in a few months.
Also, it is interesting that the Apob and non-HDL percentiles are just about identical, in this case, non-HDL constitutes an almost perfect proxy of ApoB.
3 Likes
So the conclusion is that the berberine or the statin was causing the ALT increase?
For me, my ALT fell and fatty liver cleared up (verified by ultrasound) when I started Rosuvastatin + Ezetimibe
mccoy
#37
I don’t know if I can draw a conclusion yet, the elevation in transaminases might have been caused by berberine alone or some other factors. I’ll have to repeat the analyses on this regime and then hypothesize. I may even reintroduce the statin and see what happens. It’s a luck now there are these capillary blood analyses available, a finger prick at the pharmacy, US$ 25, and you get so many parameters.
I doubt I had fatty liver, I don’t know if that’s possible with low adiposity, I estimate was about 8-10% then.