Thanks. The paper you attached describes Carnosine ability to prevent formation of AGEs not clear them up after formation. This sounds right to me, and would be useful. I think the most important tactics are to keep the glutathione system healthy, be insulin sensitive, and avoid eating AGEs. I’m not an expert in the topic but I am researching it for a podcast I’ll be doing in October.
1 Like
It’s a good suggestion. This issue I may have is that I have one kidney, so I’m wary of uric acid. MYbe it’s not as much of an issue?
I currently take NMN, but am wondering if there is a real benefit of high levels of NAD and whether actually NAD boosting can be counter productive in some circumstances.
2 Likes
Bicep
#24
I know Niacin improves kidney function. I don’t know much about Uric Acid.
1 Like
I think you are correct, and is another case of my lack of reading comprehension: the paper does say “prevent” rather than “clear”. I think I must have seen this somewhere so I’ll need to find it later (if it even exists). If you are correct, carnosine only works when administered, and does not clear prior damage. Thus we’d need to keep higher serum levels to be useful (take it forever). I’m not a fan of that.
There is this:
Carnosine Stimulates Macrophage-Mediated Clearance of Senescent Skin Cells Through Activation of the AKT2 Signaling Pathway by CD36 and RAGE - PMC.
Results: Carnosine promoted macrophage-mediated elimination of senescent skin cells in the co-culture. Through the AKT2 signaling pathway, carnosine upregulated the expression of CD36 and receptors for advanced glycation end products and elevated the phagocytic capacity of the macrophages, thereby promoting the ability of the macrophages to eliminate the senescent skin cells.
Conclusions: Carnosine could boost the immune surveillance ability of macrophages to clear senescent keratinocytes and fibroblasts in the macrophage-senescent skin cell co-culture by activating the AKT2 signaling pathway, suggesting the possibility of using carnosine as an agent to reverse skin aging.
Another possible (related) benefit:
Carnosine’s ability to reduce the formation of altered proteins (typically adducts of methylglyoxal) and enhance proteolysis of aberrant polypeptides is indicative of its influence on proteostasis. Furthermore these dual actions might provide a rationale for the use of carnosine in the treatment or prevention of diverse age-related conditions where energy metabolism or proteostasis are compromised. These include cancer, Alzheimer’s disease, Parkinson’s disease and the complications of type-2 diabetes (nephropathy, cataracts, stroke and pain), which might all benefit from knowledge of carnosine’s mode of action on human cells.
3 Likes
Bicep
#26
I have cut back from 1.5 grams to just 500mg a day. I know it’s an issue, but the test is so expensive I’m just going to be moderate in all.
1 Like
I’m aware of evidence that β-alanine increases muscle carnosine better than carnosine supplementation, but not serum carnosine. Examine.com mentions that “Carnosine cannot enter muscle cells to a significant extent, but its two substrates [β-alanine and L-histidine] can.”
However, if you’re goal is to prevent/reduce AGEs, then you want more serum carnosine—not muscle. The enzymatic reaction that produces carnosine from β-alanine and L-histidine occurs inside of cells. I’m not aware of evidence that this intracellular carnosine is then secreted into the blood. Additionally, the enzyme that catalyzes this reaction, carnosine synthase, is not (or minimally) expressed in most tissues:
(Human Protein Atlas: CARNS1)
So, β-alanine supplementation increases intracellular carnosine content in the subset of tissues that express carnosine synthase. This increase likely benefits athletic performance. But, if you want to increase serum carnosine, you’ll probably need to supplement with carnosine itself.
Here’s one piece of suggestive evidence that supports this line of reasoning:
In two-month-old Senescence Accelerated Mice (SAMP1), carnosine (100 mg/kg in drinking water) extended median lifespan by 20% while β-Alanine and L-histidine (matching their molar proportions in carnosine) had no effect (Gallant et al. 2000). The maximum lifespan of SAMP1 mice is approximately 15 months.
9 Likes
Very interesting, thank you, @McAlister . Am I reading your chart correctly? — if this is “carnosine concentrations resulting from oral beta-alanine supplementation” then I see the brain (and other nervous systems) more than skeletal muscle, and basically nothing for other organs. So not optimal (because it is NOT addressing connective tissue and blood vessels as I had thought), but addressing AGEs in brain systems seems a positive, no?
Or is your chart “organs which express carnosine kinase” in which case we’d need to cross-reference the results with “organs in which oral beta alanine reaches”
That it doesn’t penetrate the skin or retina isn’t surprising either; this would need to be added to a DMSO skin serum or the like.
The mouse results are interesting: I don’t think I saw this in the ITP. a 20% increase in lifespan for 100mg/kg per day is substantial, and I would have thought this might be covered by other labs. This is on the order of Rapamycin if confirmed, and likely a different pathway. Why aren’t others in this forum taking carnosine (and not beta-alanine) at the roughly 7.5g per day level?
Because most mice lifespan studies other than the ITP are trash.
lin
#30
@ericross2
Thanks for sharing, I think your results look good, I personally wouldn’t be too worried if I had high LDL in the context of low triglycerides, normal glucose and optimal HDL levels. Cholesterol ratios are better predictors of heart disease risk than individual readings themselves, and according to recent studies your cholesterol ratio of 3.51 would put you around the lowest hazard rate.
Chart from https://www.frontiersin.org/articles/10.3389/fendo.2022.1012383/full
I would get a CAC scan though to be safe. Recommendations are “for adults without known risks for premature heart disease, the authors say an ideal time is age 42 for men and 58 for women”. Getting the scan would be even more prudent if you have high cholesterol and are above the recommended age.
1 Like
Plenty of cardiologists would disagree with this advice.
lin
#32
Those are good observations, there is no carnosine transporter across the blood brain barrier (L-histidine and L-carnosine exert anti-brain aging effects in D-galactose-induced aged neuronal cells - PMC). From the chart, the highest levels of carnosine synthase are expressed in neuronal tissue that may have limited exposure to serum carnosine, so beta-alanine supplementation may still be important.
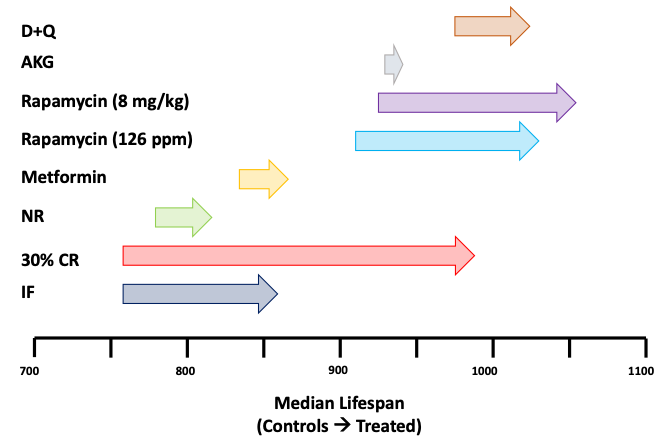
That Russian study is over 20 years old using short-lived control mice with roughly half the lifespan of mice used in the rapamycin studies. If we were to try to plot this study on Kaeberlain’s graph (https://twitter.com/mkaeberlein/status/1510699077414973440?lang=en)… we wouldn’t be able to because the plot would be far off to the left end.
For these results to have credence, I’d really want to see some level of (higher quality) replication in the 2 decades or so since that study was published.
Personally I think beta-alanine/carnosine are worthy of an ITP trial, but as it is there’s a dearth of studies of their effects on lifespan, especially given their putative roles in aging.
4 Likes
lin
#33
The only advice I gave was to get a CAC scan
1 Like
The chart I included shows the presence of carnosine synthase (an enzyme) across different organs, quantified at the RNA level. It represents the organs capable of forming carnosine from the precursors β-alanine and histidine. It is not a readout of carnosine concentrations.
AGEs form both intracellularly and extracellularly, so it’s at least plausible that dietary β-alanine could affect intracellular AGE formation by supporting the production of intracellular carnosine in a subset of organs.
As for the (Gallant et al. 2000) study, there are two major caveats:
-
These are short-lived mice: ~15 month maximum lifespan vs. ~36 month maximum lifespan in C57BL/6 mice. The presence of lifespan extension in short-lived mouse models can direct us to some interesting underlying biology, but the magnitude of the extension is often not informative. @lin posted Matt Kaeberlein’s helpful explanation of this topic above.
- Compared to the ITP, this is a small study (n = 36). It’s plenty large enough to make statistically significant comparisons, though.
I do not expect carnosine to extend lifespan by 20%. My takeaway from this study was that supplemental carnosine has effects in the body that supplemental β-alanine and L-histidine do not. The limited tissue distribution of carnosine synthase provides a rationale for that result.
Lastly a 100 mg/kg dose in mice does not scale linearly to human doses. The human equivalent dose (HED) for mice of this size is 100 mg/kg ÷ 12.3 = 8.13 mg/kg → 570 mg HED70 (Nair and Jacob 2016).
6 Likes
Fair enough. I was looking at this comment, which was not advice, as you say.
1 Like
lin
#36
Correct, that is an expression of personal opinion, which I thought “personally” would make abundantly clear.
Now that you’re taking me down this route, what’s your source for your claim that “most cardiologists” would disagree?
1 Like
My totally anecdotal observations: I have been visiting cardiologists once a year for decades, and not once has one even suggested that I get a CAC scan. In addition, none of my insurance companies would pay for it. Why is that? I believe they are of limited value in most cases.
3 Likes
The best advice would be to start high dose atorva/rosuvastatin and ezetimibe first, do an apoB test a few months later and then reevaluate 
2 Likes
I might argue that health insurance companies would far rather see us die quickly via sudden CVD from atherosclerosis rather than hang on for decades requiring insurance costs. Thus not paying for a CAC score makes sense in this cold-hearted logic.
It’s the opposite for life insurance companies, of course: they’d rather you hung on to life, miserable but alive.
3 Likes
For clarity, I said “plenty” of cardiologists would disagree. I follow several well known cardiologists/ lipidologists on Twitter who always say to look at apoB and that ratios are not useful. The only name I can recall is Thomas Dayspring, who has been a guest on many popular podcasts over the past few years. He seems credible to me. What is the source of your opinion?
1 Like