JuanDaw
#1744
Try probenecid.
https://www.drugs.com/compare/allopurinol-vs-probenecid
Allopurinol has an average rating of 7.4 out of 10 from a total of 91 ratings on Drugs.com. 64% of reviewers reported a positive effect, while 20% reported a negative effect.
Probenecid has an average rating of 9.7 out of 10 from a total of 7 ratings on Drugs.com. 100% of reviewers reported a positive effect, while 0% reported a negative effect.
https://www.jacc.org/doi/10.1016/j.jacc.2017.12.052
In this large cohort of 38,888 elderly gout patients, treatment with probenecid appears to be associated with a modestly decreased risk of CV events including MI, stroke, and HF exacerbation compared with allopurinol.
1 Like
The commentary is really interesting, and does a good job of balancing the strengths of the study and the wider knowledge in the field. I am personally not yet ready to be convinced that Lp(a) isn’t a risk factor, but, it’s clearly not a simple 1 = 1 type relationship where higher is guaranteed to be worse. That’s good news for somebody like me who fits the demographics of this paper quite well (younger, male, and I’d be in Q5 for Lp(a)).
As we know, some people have horrible circulating lipids but keep a low atherosclerotic burden their whole lives, whereas other people steadily build plaque with ApoB levels of 70mg/dl. There’s a huge amount of factors which go into plaque accumulation, regression and calcification, not just your circulating lipid concentrations. It’s really interesting to see more nuance being added to the overall picture.
Neo
#1746
100%
And that paper is only really discussing CAC
Not other risks like how Lp(a) contributes to calcification of the aortic valve, leading to aortic stenosis, or thrombosis formation risks.
2 Likes
How would you diagnose the “calcification of the aortic valve”? Wouldn’t that show up in a CAC scan? So “discussing CAC” should cover that, no? What am I missing?
I ask, because I’ve had very high LDL all my life (and ApoB, as measured more recently), and also aky high Lp(a). I’ve only been on a low dose atorvastatin (10mg/day) for a little over five years. Yet, I had a CAC scan at age 65, and the score was zero. Of course I might have a lot of soft plaque. But the point being, is if we are talking about atherosclerosis impacted by Lp(a), how else would you discuss it other than in the context of CAC or angiogram.
1 Like
Neo
#1748
Good question: I looked into it a bit more and the answer is hopefully yes, but perhaps not it seems:
4o:
When radiologists interpret a CAC scan (or any cardiac CT), their primary task is to evaluate coronary calcification. However, they should also examine the aortic valve for calcifications. In the past, incidental valve calcium was often underreported - mild calcification might be overlooked or simply not mentioned in the official report . The focus used to be on coronary arteries, and unless the valve calcification was very pronounced, it might not make it into the summary.
Today, there is growing awareness that aortic valve calcification is clinically important. Consensus recommendations now urge radiologists to report any significant aortic valve calcification seen on routine chest CT scans (including CAC scans) . The British Society of Cardiovascular Imaging, for example, recommends that whenever the heart is visible on a CT (even one done for non-cardiac reasons), the reader should note calcifications in the coronary arteries and aortic valve . On a CAC scan report, a radiologist may add a line such as “Aortic valve calcification present” and often will qualitatively describe it (e.g. “mild,” “moderate,” or “severe”). There isn’t usually a numeric score given for the valve in routine practice, but if the calcification is heavy, some centers might quantify it or at least flag it.
(The general point that Lp(a) is risky for other reasons that normal arterial plack is still my main point)
Interesting. This is a quote from my December 2023 CAC scan at UCLA:
"FINDINGS:
Coronary artery calcification present in 0 vessels and the total CAC score is 0. The calcium score for each vessel is as follows:
Left main = 0
Left anterior descending = 0
Left circumflex = 0
Right coronary artery = 0
The ascending aorta measures 29 mm, which is normal. No aortic valve leaflet calcifications. No atherosclerotic calcifications of the partially visualized thoracic aorta."
I take the sentence: “No aortic valve leaflet calcifications.” to mean that they did in fact look for calcifications of the aortic valve.
If that is so, then it seems that Lp(a) impact on the aortic valve calcification can be assessed through a CAC scan.
2 Likes
A_User
#1750
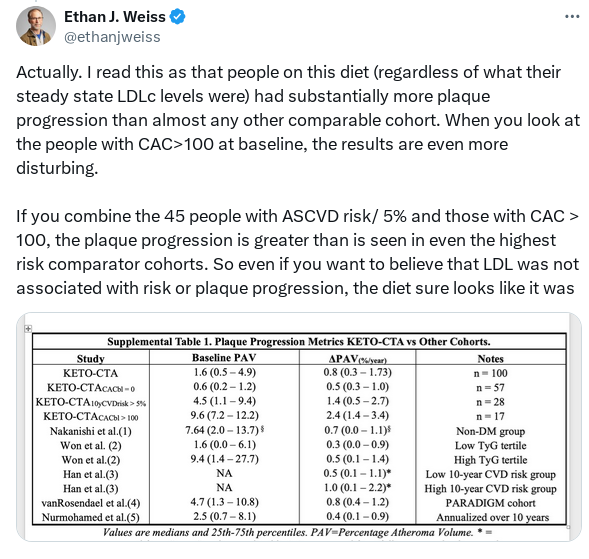
Something is very off about the communication about the KETO-CTA study, it’s the regular old bias probably, in this case bias that is expected to get people killed.
Didn’t report the primary outcome in the study:
From Ethan Weiss (non-ideological keto dieter)
https://x.com/ethanjweiss/status/1909686881425801227#m
It all just stinks ideology, having a conclusion and making the data fit it, I don’t mean this study but ALL data that exists on apoB and ASCVD progression. Missing the forest for the trees, not knowing, ignoring, or not understanding EXPECTED VALUE and reasoning under uncertainty.
But sure, plaque progression in metabolically healthy keto dieters is the same or WORSE than unhealthy cohorts (like Weiss pointed out), and much more disturbing at >100 CAC. What’s prevention of ASCVD? Where’s the reporting of the primary outcome as mentioned on ClinicalTrials.gov?
It’s pretty disturbing from an expected value perspective, but whatever.
3 Likes
My question is, what would I do differently if I got a bad score?
The answer is nothing.
Being in the lower-the-lipids camp, I am already acting like I got a bad score.
I take atorvastatin and Brillo EZ. All of my lipids are in the low range except for HDL.
6 Likes
CAC/CTCA can be helpful evidence to support insurance coverage, particularly of PCSK9-inhibitors, which can’t be sourced from India. Otherwise, agreed, if you’re already urgently lowering lipids and a positive scan won’t change your strategy, probably not much value.
2 Likes
A_User
#1754
Can’t you monitor soft plaque progression with CTCA? Genuinely curious.
1 Like
Yes. Also could decide to intervene with stents or other surgery based on it.
4 Likes
A_User
#1756
But I haven’t heard about anyone measuring efficacy of therapy or otherwise based on routine monitoring with CTCA. I’m thinking of e.g the case of someone who is still developing plaque at a low apoB and might e.g decide to lower it even further.
Like 99% have positive CAC eventually so might be important to be ahead on this.
1 Like
A_User
#1758
Arresting the primary cause of death.
If you get +18mm3 over 1 year - no points!
Beth
#1759
I’m interested to know what you know about this.
I’ve considered getting the CLEERLY but I consulted with my soon to be ex cardiologist and my future cardiologist and they both told me that they don’t do preventative stents unless their patient is having symptoms. ?
A_User
#1760
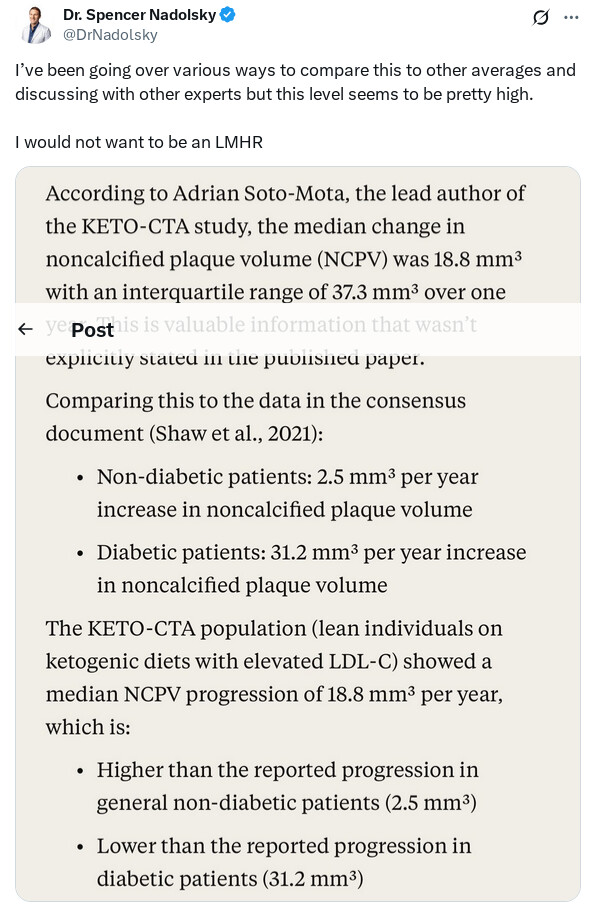
LMHR 7 times higher than a non-diabetic patient (2.5 mm3 vs. 18.8 mm3) and half the progression as in diabetic patients (18.8 mm3 vs. 31.2 mm3).
3 Likes
Bicep
#1761
You don’t have to get a stent to have the CTCA. My sister just got 2 of them done and they found some blockage, but said it wasn’t much so they let her go. People do them for the Cleerly all the time just because they want to know. I nearly did, but could not find out the rate of adverse events for a CTCA in a healthy person. I’m sure it depends on the skill of the team and of course I live in the sticks.
Also there are companies that do it without a doctors order. It’s about $500 here. Probably if the doc orders it for you then it’s covered, but the Cleerly isn’t and it’s more like $1200 here
2 Likes
It would probably be whatever the rate of adverse events is for the contrast agent, which is typically iodine. Also the radiation dose. I doubt there’s anything specific to a CTCA regarding adverse events otherwise.
1 Like
I don’t know much about this, but a quick search shows
The primary endpoint of target vessel failure at 2 years (composite of death from cardiac causes, target vessel myocardial infarction [TV-MI], ischemia-driven target-vessel revascularization [ID-TLR], or hospitalization for unstable or progressive angina) for PCI + OMT vs. OMT alone, was: 0.4% vs. 3.4% (hazard ratio [HR] 0.11, 95% confidence interval [CI] 0.03-0.36, p = 0.0003).
Target vessel failure at 7 years: 6.5% vs. 9.4% (HR 0.54, 95% CI 0.33-0.87, p = 0.0097)
Key secondary outcomes for PCI + OMT vs. OMT:
- All-cause mortality at 2 years: 0.5% vs. 1.3%, p > 0.05
- All-cause mortality at 7 years: 5.2% vs. 7.4%, p > 0.05
- All MI at 2 years: 1.1% vs. 1.7%, p > 0.05
- All MI at 7 years: 2.4% vs. 3.5%, p > 0.05
- ID-TLR at 2 years: 0.1% vs. 2.4%, p < 0.05
- ID-TLR at 7 years: 4.9% vs. 8.0%, p < 0.05
- All-cause mortality or TV-MI at 2 years: 0.6% vs. 1.9%, p < 0.05
- All-cause mortality or TV-MI at 7 years: 6.2% vs. 8.6%, p > 0.05
These HRs and comparisons seem quite impressive.
The results of this trial suggest that PCI of focal non-FFR-positive plaques that are angiographically >50% and have evidence of vulnerability on intravascular imaging (preventive PCI) along with OMT is superior to OMT for clinical outcomes at 2 years among patients with predominantly SIHD
Symptoms was not one of the inclusion criteria.
Seems like the cardiologists you spoke to are out of date? Or perhaps they meant they refer out preventative work?
1 Like