The incidence of certain autoimmune diseases in our society, including multiple sclerosis and type 1 diabetes, has been rising over recent decades. This research suggests that one factor may be that we now eat more processed foods with high levels of salt.
“It’s premature to say, ‘You shouldn’t eat salt because you’ll get an autoimmune disease.’” Regev says. “We’re putting forth an interesting hypothesis — a connection between salt and autoimmunity — that now must be tested through careful epidemiological studies in humans.”
“Once we have a more nuanced understanding of the development of the pathogenic Th17 cells, we may be able to pursue ways to regulate them or their function,” Kuchroo adds.
Hafler’s group has begun preliminary studies to determine whether restricting salt intake can influence autoimmune disease in people. Hafler says, “I have already begun to suggest to my patients with multiple sclerosis that it may not be bad to restrict their dietary salt intake.”
As reported in the January 20, 2010, online edition of the New England Journal of Medicine, the scientists found that reducing salt intake by 3 grams per day could cut the number of new cases of coronary heart disease each year by as many as 120,000, stroke by 66,000 and heart attack by nearly 100,000. It could also prevent up to 92,000 deaths each year. All segments of the population would benefit, with African-Americans having the greatest improvements overall. Women would particularly benefit from reductions in stroke, older adults from reductions in coronary heart disease and younger adults from lower mortality rates.
Reducing salt intake by 3 grams per day would save the country up to $24 billion in health care costs a year, the researchers estimated. Even a modest reduction of 1 gram per day between 2010 and 2019 would be more cost-effective than using medications to lower blood pressure in people with high blood pressure.
“Our study suggests that the food industry and those who regulate it could contribute substantially to the health of the nation by working toward reducing the amount of salt in the processed foods that all of us consume,” Bibbins-Domingo says.
Normal BP is below 120/80.
Controlling your blood pressure can help prevent or delay serious health problems such as chronic kidney disease, heart attack, heart failure, stroke, and possibly vascular dementia.
It’s so recent knowledge that sodium is stored in bones I could only find a rap video.
In classical physiological teaching, ingested sodium (combined with inadequate excretion) leads to expansion of the extracellular water compartment, congestion, and increasing blood pressure.4 This model is now being augmented with additional appreciation of retained sodium being stored without associated water, within skin, muscle, and bone.
Stored sodium is not biologically inert and can result in a variety of pathophysiological consequences. Preclinical data suggest that sodium may be directly deposited in myocardium and vascular structures leading to tissue remodeling and inflammation. This is independent from the well-described effects of pressure and volume overload.
This study has some inherent limitations. First, we were not able to assess clinical impact of salt removal, especially the relationship between skin sodium storage and direct myocardial effect. Moreover, we did not provide causalities or correlation with mortality. We reported in this present study a preliminary exploratory study on tissue sodium storage and emphasized what 23NaMRI could offer to clinical care of HF patients. We would need to increase the number of sampled patients to reach a higher level of certainty. A longitudinal study would be also needed to assess impact of skin sodium storage on cardiovascular events in a future study.
In conclusion, excessive nonosmotically active tissue sodium storage seems to be a characteristic feature of severe HF, over and above any associated renal impairment. Evolving appreciation of the direct toxic consequences of tissue sodium (including myocardial deposition and cardiac fibrosis), developing access to pharmacological and direct dialytic sodium removal strategies highlight the importance of sodium homeostasis in HF and the potential role for 23NaMRI in the management of large and challenging group of patients with HF.
https://www.ahajournals.org/doi/full/10.1161/CIRCIMAGING.121.012910
SODIUM MRI
Recently, we used 23Na-MRI in AD patients on a ultra-high-field (7 T) MR scanner, and were able to show sodium increases in several brain regions, associated with tau-pathology assessed by Flortaucipir-PET imaging in AD (Haeger et al., 2021).
A total of 86 subjects, comprising 52 patients with AD (20 female, mean age 70.4 ± 6.1 years), 20 age-matched elderly control subjects (4 female, mean age 67.8 ± 9.4 years) as well as 14 younger control subjects for analysis of age-related effects (5 female, mean age 29.2 ± 6.4 years) participated in the study.
Interestingly, TSC [Tissue Sodium Concentration] is strongly age- and volume-driven and is linked to the cognitive decline of patients. TSC might therefore serve as a potential marker of cellular energy depletion and disturbed homeostasis, associated with the different states of cognitive decline. TSC could therefore be useful in clinical trials for the evaluation of intervention effects, with a potential metabolic focus.
https://www.sciencedirect.com/science/article/pii/S2213158222003394
Prehistoric man was characteristically exposed to very low levels of dietary sodium—typically with 20 times higher potassium than sodium in their urine (sodium/potassium ratio 0.02); life expectancy reached 70 years and modern day non-communicable diseases such as heart attacks and strokes were almost absent [2]. In stark contrast, we can find urinary sodium/potassium ratios of 10 (healthy < 2.4) in youth with kidney stones [3]. Diseases that used to be described in adults such as hypertension, kidney stones, type II diabetes, metabolic syndrome, and even cardiovascular disease are increasing among adolescents and young adults (AYA) [4,5,6,7]—all potentially linked to increased sodium exposure.
The gap between rich and poor is increasing in developed countries, and in view of the detrimental impact of high salt diet in childhood on longevity and all-cause mortality, we need a call to action.
Too much salt is already a problem since salt worsens the edema of the face, hands, legs, ankles, and feet commonly experienced by the mother during pregnancy. Moreover, high maternal salt intake affects the fetal renal renin angiotensin aldosterone system (RAAS). According to the Dietary Guidelines for Americans established by the Department of Agriculture and the Department of Health and Human Services, the recommendation is up to about a teaspoon of salt a day—that is, 6 g of salt, or approximately 2300 mg of sodium. However, most people living in North America consume more than 3500 mg of sodium per day, including pregnant women
The developmental origins of health and disease theory indicates that many adult-onset diseases originate in the earliest stages of life. The developing kidney is particularly vulnerable to adverse in utero conditions, leading to morphological and functional changes and potentially suboptimal nephron endowment. Malnutrition is the common factor related to hypertension and kidney disease; however, a variety of nutritional insults can cause renal programming including high sucrose and fructose consumption, protein and calorie restriction, and high fat diet [13]. High salt diet during pregnancy needs to be added to this list, at least suggested by data derived from experimental study of female Wistar rats [13, 14]. Oxidative stress, an imbalance between reactive oxygen/nitrogen species and antioxidant systems, plays a pathogenic role in the developmental programming of kidney disease [15]. There is increasing evidence that activation of the RAAS increases oxidative stress. This is important since there is a finite nephron endowment that develops until 36 weeks of gestational age [16].
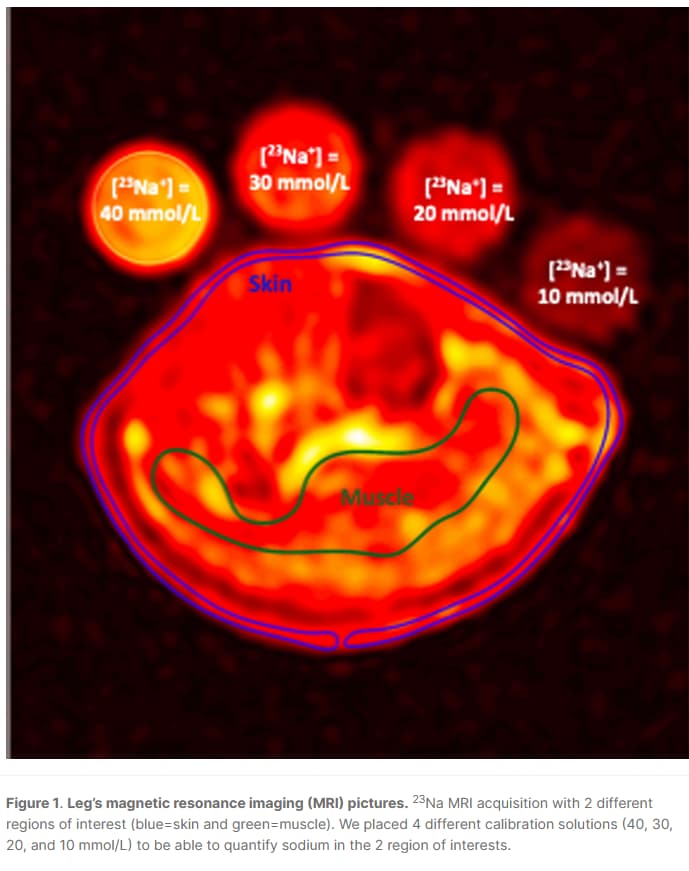
Healthy children (n = 17) had a median skin sodium concentration of 13.4 (3.3 interquartile range [IQR]), whereas 19 healthy adults had a median skin sodium concentration of 18.7 (6.2 IQR). Similarly, muscleSoleus sodium concentrations were 18.6(1.6 IQR) in children and 22.2 (4.3 IQR) in adults (unpublished results). Sodium concentrations correlated with age.
Tissue sodium has been shown to be mobilized by loop diuretic therapy [27], hemodialysis [28], and the novel sodium glucose cotransporter 2 (SGLT2) inhibitors [29•]. SGLT2 inhibitors are a class of drug widely used in the management of type 2 diabetes mellitus that work by inhibiting the reabsorption of glucose in the proximal convoluted tubule [30]. This class of medications inhibits the coupled reabsorption of sodium and glucose, thereby increasing urinary sodium and glucose wasting. The natriuretic effects coupled with tissue sodium depletion may be one of the main reasons why these medications have such a profound effect on cardiovascular complications [31].
USD is a critical public health concern as it is associated with osteoporosis, the development of CKD, and shortened life-expectancy [42, 43]. A large proportion of USD patients already developed decreased bone mineral density [**44, 45]. Interestingly, this was more prevalent in adolescent males [46], even though females tend to have lower bone mineral density z-scores than males. A major reason for USD is the steady increase in dietary sodium intake in Western countries (typically > 3500 mg/day, whereas the World Health Organization (WHO) recommends < 2000 mg/day) [11, 12, 47, 48]… There is a direct relationship between urinary sodium excretion and urinary calcium wasting [50]. This makes limiting the salt intake the easiest step to reduce the lithogenic risk [
“The sodium intake in the USA for children aged 6–11 years of age increased from 200 mg/day in the 1970s to 3000 mg/day in the 2000s [49]”
This review highlights the relationship between high salt intake and chronic life-limiting conditions such as hypertension, USD, osteoporosis, and CKD in children and AYA as well as the importance of sodium accumulation in the body, measured by 23Na MRI of muscle and skin. The high salt diet in Western societies may be the easiest modifiable factor to curb the growing prevalence of these non-communicable diseases. Obviously, salt wasters must be identified and supplemented accordingly. We exhort the reader to engage in advocacy efforts to curb the incidence and reduce the prevalence of high salt-related life-limiting conditions.