Rhonda Patrick of FoundMyFitness sends an email Newsletter to my inbox - The following cut/pasted from my email: Jan 16, 2025: The Case for Vitamin D in Dementia Prevention Well written and compelling reading (not sure about the accuracy of the science reporting).

Vitamin D isn’t just a vitamin—it’s a hormone that controls thousands of genes in the human body, many of which are in the brain.
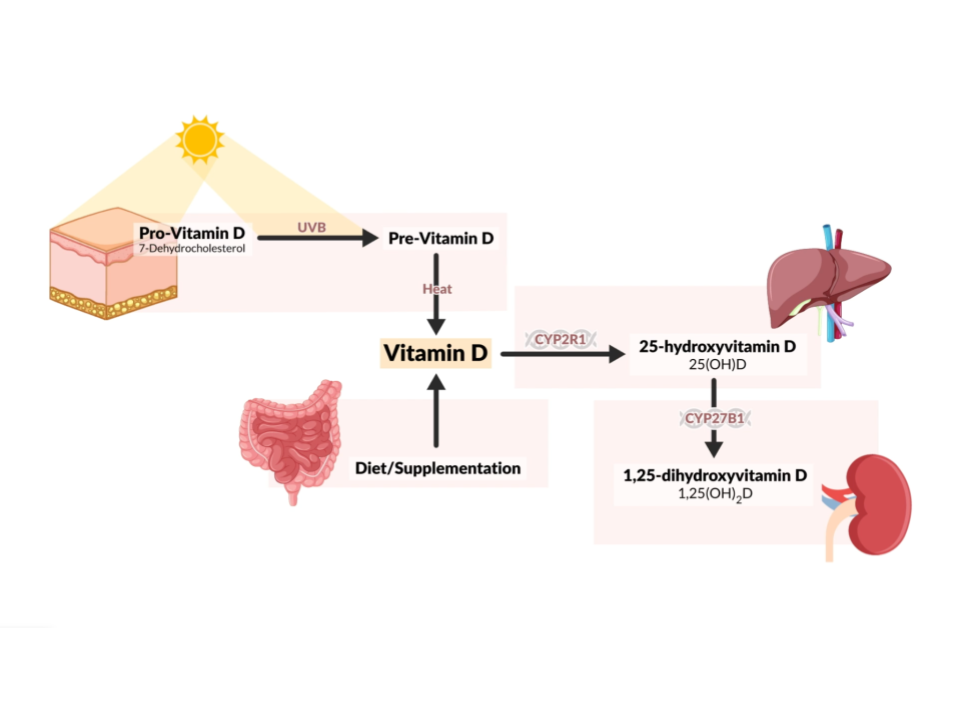
The primary source of vitamin D is UVB radiation from the sun—which our skin uses to synthesize vitamin D3. Insufficient sun exposure, season changes in UVB, aging, and body weight can all affect our ability to produce vitamin D and its bioavailability. Because nearly 70% of the population has insufficient levels of vitamin D (blood levels <30 ng/mL) and a large percentage have deficient levels (<20 ng/mL), supplementing with vitamin D makes sense for most!
This might be especially true if you’re concerned about dementia risk (as we all should be).
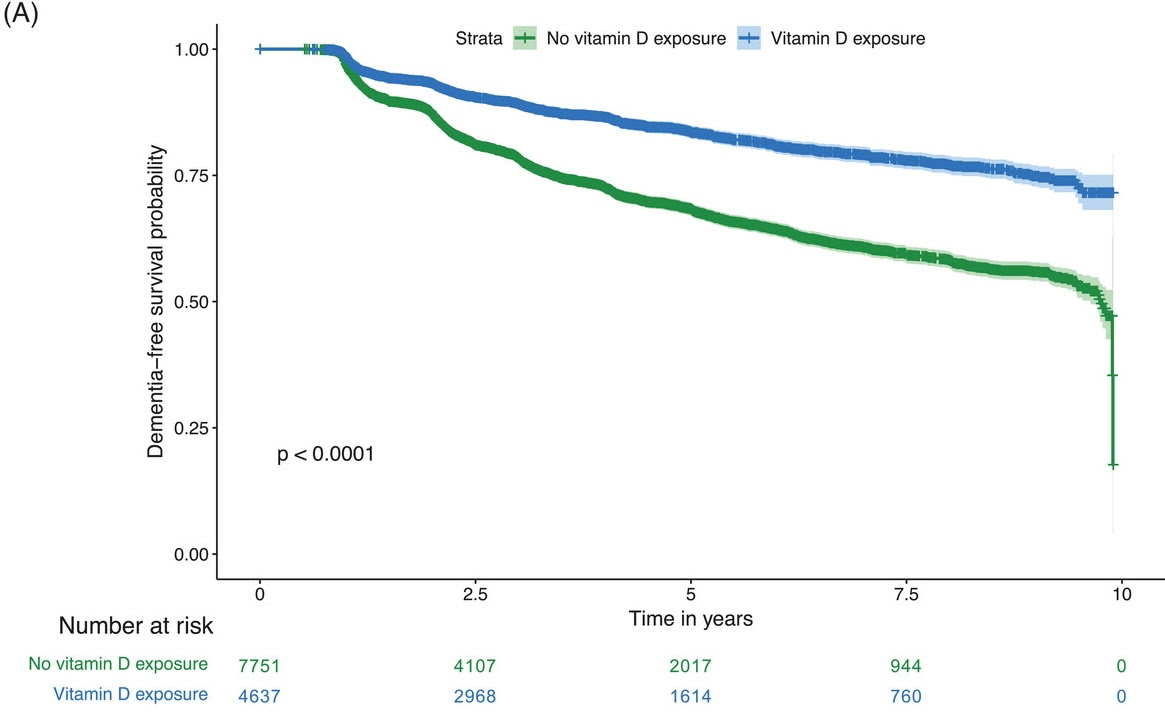
In a study of over 12,000 dementia-free adults, those who used vitamin D had a 40% lower risk of dementia over a decade.
Remarkably, 84% of supplement users were dementia-free after five years, compared to just 68% of non-users. The benefits of vitamin D even extended to high-risk groups: In adults with mild cognitive impairment (MCI) and those who carried one or two copies of the APOE e4 allele—a major risk factor for neurodegenerative diseases—the risk of dementia was 33% lower compared to adults with MCI/APOE e4 carriers who didn’t use vitamin D.
While vitamin D reduced dementia risk across the board, some groups benefitted more.
Women, adults with normal cognition, APOE e4 non-carriers, and those without depression saw the greatest brain-protective effects from vitamin D supplementation.
Regardless of sex, genetic risk, or baseline cognition, the evidence is clear: Vitamin D is a powerful ally in reducing dementia risk. Though dosage details and optimal blood levels remain unknown, the link between vitamin D and brain health is too significant to ignore.
In today’s email, we’ll explore the importance of vitamin D for brain and body health and break down this study in more detail. I’ll also provide some practical takeaways about vitamin D supplementation.
Why Vitamin D Benefits the Brain
Vitamin D is linked to several benefits for human health.
-
Supports neurodevelopment: High-dose vitamin D supplementation in early childhood reduces the risk of internalizing behaviors such as depression and anxiety, especially in children with low prenatal vitamin D exposure.
-
Enhances brain function synergistically with exercise: Vitamin D supplementation combined with exercise improves functional brain connectivity in regions associated with memory and cognition.
-
Improves muscle strength and mass: Higher vitamin D levels enhance muscle strength and mass while reducing fat mass, likely through metabolic and hormonal pathways.
-
Promotes tooth remineralization: Vitamin D supplementation increases calcium and phosphorus in teeth, reducing the risk of demineralization and cavities.
-
Supports healthy aging: Vitamin D maintains genomic stability, mitochondrial function, and reduces cellular senescence, mitigating the hallmarks of aging.
-
Facilitates calcium homeostasis and bone health: Vitamin D regulates calcium absorption and bone remodeling, reducing the risk of osteoporosis and fractures, especially in aging populations.
Higher levels of vitamin D have also been associated with lower odds of dementia and mild cognitive impairment (MCI), better cognitive function, a reduction in Alzheimer’s disease risk, and larger total brain, gray matter, and hippocampal volumes.
How might vitamin D protect against dementia and Alzheimer’s?
Vitamin D helps clear amyloid beta aggregates which are considered to be one of the hallmarks of Alzheimer’s disease. It also appears to target another hallmark of Alzheimer’s disease—tau protein hyperphosphorylation. These effects have been attributed to less reactive oxygen species production, greater immune system clearance of amyloid beta proteins, and an increase in glial cell line-derived neurotrophic factor or GDNF—a brain protein that helps neurons survive and regenerate.
A 12-month randomized controlled trial found that vitamin D supplementation improved cognitive function, intelligence quotient scores, telomere length, and lowered oxidative stress markers in older adults with mild cognitive impairment (compared to placebo), suggesting that not only does vitamin D supplementation improve biomarkers of aging, but also functional outcomes.
Even though the study we’ll discuss today didn’t investigate these mechanisms, its results are still a testament to the importance of vitamin D for neurological health, especially later in life.
Quick pause! These weekly email deep dives are made possible by the generous contributions of FoundMyFitness members. I warmly invite you to become a Premium Member today. For just $15/month, you’ll gain access to everything we offer while helping us fulfill our mission of making science accessible to all! Learn more at the bottom of this email or by clicking the button below.
Become a Premium Member today!
Supplementing with Vitamin D Reduces Dementia Risk
The study included 12,388 adults who were divided into two groups: Those who reported using vitamin D supplements in any form (calcium-vitamin D, ergocalciferol/vitamin D2, or cholecalciferol/vitamin D3) and those who didn’t.
During the 10-year follow-up period, supplementing with vitamin D was associated with a 40% lower incidence of dementia: Over 2,000 participants who reported never using vitamin D supplements developed dementia compared to just 679 of those who used vitamin D.
Supplementing with vitamin D was also associated with a greater 5-year dementia-free survival—84% of adults in the vitamin D group were free of dementia during this time period while only 68% of the non users were dementia-free.
This was also true regardless of whether or not the participants had baseline MCI or normal cognitive function—vitamin D provided a benefit in both cases. While dementia prevalence was higher in adults with MCI, it was around 15% lower in this group for adults who supplemented with vitamin D compared to those who didn’t.
Some populations benefit more
Although vitamin D supplementation reduced dementia risk among all groups, there were several interesting findings regarding the benefits of vitamin D for certain populations:
-
Women derived a greater benefit from vitamin D: They experienced less dementia compared to men who supplemented. Furthermore, while vitamin D-using men had a 26% lower dementia incidence than non-using men, vitamin D-using women had a 49% lower incidence compared to non-using women.
-
Adults with normal baseline cognitive function had a 56% lower dementia incidence if they supplemented with vitamin D; however, adults with MCI had only a 33% lower incidence if they supplemented.
-
Among APOE e4 carriers, supplementing with vitamin D reduced the incidence of dementia by 33%, and among non-carriers, vitamin D reduced the incidence of dementia by 47%. Furthermore, among APOE e4 non-carriers, vitamin D use was associated with a 47% reduction in dementia incidence, while among carriers, vitamin D only mitigated dementia incidence by 33%.
Supplementing with vitamin D wasn’t enough to outweigh the effects of carrying one or two copies of the APOE e4 allele—these participants still had a 16% greater risk of dementia than non-carriers, even non-carriers who didn’t use vitamin D. The same was true for another risk factor—having MCI—which elevated dementia incidence by nearly 400% compared to having normal cognition, even in the presence of vitamin D supplementation.
Slowing the Decline for Those with Cognitive Impairment
Participants with MCI who didn’t supplement with vitamin D had more than a 600% increase in dementia risk compared to adults with normal cognitive function, even those who didn’t use vitamin D. But having MCI and supplementing with vitamin D offered some risk reduction—these participants’ dementia risk was 390% higher than adults with normal cognitive function—still high, but not as bad as having MCI and not using vitamin D!
It didn’t matter the form of vitamin D used—all of them were associated with a lower dementia risk. Specifically, using calcium-vitamin D was associated with a 44% lower dementia risk, using cholecalciferol (vitamin D3) was associated with a 37% lower risk, and ergocalciferol (vitamin D2) was associated with a 50% lower risk. Using combined forms of vitamin D was associated with a 50% lower risk.
Final Thoughts
These findings give strong support to the idea that everyone should probably be supplementing with at least some vitamin D to support optimal brain health.
This is especially true if you are exposed to risk factors for dementia like having one or more copies of the APOE e4 allele, mild cognitive impairment (or a family history of it), and others that weren’t investigated in this study like high blood pressure or metabolic dysfunction.
However, it is also important to note several caveats that warrant consideration. First, this was not a randomized controlled trial but an observational study, which introduces the potential for healthy user bias—adults who take supplements like vitamin D may also engage in other health-promoting behaviors that reduce dementia risk, independently of the supplement itself. Additionally, the study did not measure blood levels of vitamin D, so we lack insight into whether the observed effects were tied to correcting a deficiency or achieving a specific target range. Lastly, we don’t know the dose of vitamin D that was associated with health improvements—just whether participants used or didn’t use vitamin D supplements.
For these reasons, we can’t definitively say that vitamin D is certain to prevent dementia. But that doesn’t negate its critical importance for health. On that note, are some important and practical takeaways regarding vitamin D and your health.

-
Natural sunlight vs. supplementation: While sunlight exposure helps the body naturally regulate vitamin D synthesis, there is a natural built-in mechanism to prevent the body from producing too much vitamin D when in sunlight. This prevents toxicity.
-
Safe supplementation: Levels above 60 ng/mL of vitamin D are likely safe for most people. Levels up to 80 ng/mL have been shown to be associated with lower all-cause mortality, suggesting a beneficial range. Going above 80 ng/mL should be done with caution.
-
Avoiding toxicity: While vitamin D toxicity can occur with very high levels (especially through supplementation), a high dose taken daily for a long time is typically required to reach toxic levels. Commonly, it’s harder to reach toxic levels with moderate supplementation, and it’s unlikely unless extreme doses are taken consistently.
-
Consider your individual needs: Some people, particularly those with genetic factors (e.g., certain SNPs), may require higher doses to maintain optimal vitamin D levels. For example, some individuals may need 5,000 to 7,000 IU per day to reach levels of 30–40 ng/mL.
-
Standard doses probably aren’t sufficient: Large-scale studies often use standard low doses (e.g., 2,000 IU), but the results are inconclusive, particularly when participants’ starting levels aren’t considered. A better approach would be to adjust the dose to individual needs, aiming for higher target levels (e.g., 60 ng/mL or higher).
-
Monitoring blood levels: If you’re supplementing with vitamin D, monitor your blood levels regularly to ensure you’re maintaining an optimal range. If you’re aiming to achieve the highest levels safely, aim for levels between 60–80 ng/mL as these have shown potential benefits without the risks associated with high toxicity. However, always adjust based on personal needs and health factors, and consult a healthcare provider for personalized recommendations.
-
Avoid deficiency: Vitamin D levels below 30 ng/mL are considered insufficient, and levels above 40 ng/mL are generally beneficial for overall health. Vitamin D deficiency occurs at a blood level below 20 ng/mL.
Interested in learning more about vitamin D and Rhonda’s current supplement routine? Check out these member-only Q&A episodes with detailed show notes that we’ve hand-picked to accompany this newsletter.