What dose do you usually prescribe?
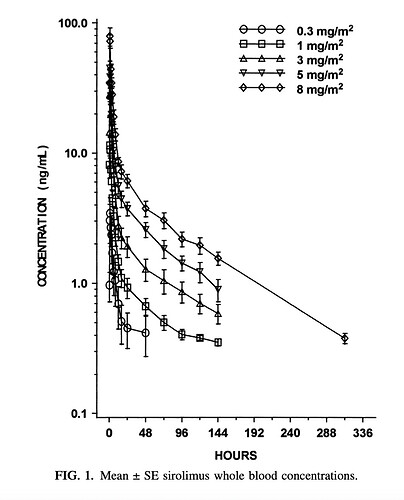
Considering the pharmacokinetics of rapamycin, the metabolism follows a pattern similar to the graph below: a high spike after ingestion followed by a rapid decline. If you aim to achieve a level of 5-6 ng/ml after 48 hours, you would likely need to administer around 12 mg as a single dose. Am I mistaken in this assumption?
1 Like
No I’m usually goaling for 5-6 at 20-24 hrs, so under the 3 ng/mL within another 48 hrs after initial measurement - but without measuring, everyone is different. Formulation, how it is taken, body weight, then metabolism. Without measuring, one really can’t be sure - some people may be 6 mg, some can be even over 12 mg. I’m still getting my experience with how people are coming in with this. Another year, I’ll have enough data. Naturally the question will be “where is your evidence?”
This is theoretic, and it makes sense to me to have a period of time over the 3 ng/mL, and have a period of recovery.
Not so interested in restarting the debate with individuals who see it differently - this is simply my approach and my logic for it.
5 Likes
Great… better make a video in YouTube to monetize it. What else happened?
Why do you believe recovery is necessary? I appreciate your perspective as a physician, emphasizing the primum non nocere principle as you mentioned in your previous post. However, my inquiry is not from a medical standpoint but rather as a user of rapamycin. I’m curious to understand your reasoning behind the necessity for recovery, considering that rapamycin only partially inhibits mTOR rather than completely blocking it. Essentially, everything slows down with rapamycin but doesn’t come to a halt. While I understand the principle of cycling drugs that block certain pathways to avoid potential harm, reaping benefits from blocking them for a specific duration, I’m interested to know if your stance on recovery aligns with this or if there’s a different rationale behind it.
2 Likes
If you take a look at the side effects of sirolimus, they are extensive. All of this however in the context of continuous use. Albeit, nuanced by the confounder that they are not usually taken in isolation and usually taken in individuals with organ transplants. However, many of them are likely from continuous dosing with continuous inhibition of mTOR. I also don’t see much evidence supporting lack of sarcopenia/osteoporosis with continuous dosing, whereas we have reasonable information indicating cyclic dosing of rapamycin, if anything is protective. If encouraging this, which is the worry with continuous dosing, this further would be a mortality risk, independent of all the other side effects that are well documented with continuous dosing.
Until I see a good amount of evidence and experience indicating a low risk side effect profile for continuous dosing, I’m certainly not going to Rx it that way. Additionally, I cannot really separate out what I do medically versus personally. I don’t personally take risks that I’d not be comfortable prescribing for the appropriate individual. I’ll let others jump in and have a go at pushing the limits and see what happens.
This is already on the threshold of my comfort level for prescribing. It also is in the context of making sure everything else possible, that has high level evidence is optimized. The vast majority of my patients are not on Rapamycin.
6 Likes
Jonas
#66
DrFraser:
the side effects of continuous dosing are mainly from transplant patients at much higher daily doses? If yes then comparing the sick population with the healthy population on continuous dosing would skew the data significantly. And the dosing would also be lower for longevity users?
Is there any data showing continuous low dosing like this by the Buck scientist is harming a healthy population? Are there any biomarkers or blood work done by healthy rapamycin users showing it is vastly inferior to high weekly dosing?
Also, the much-worshiped Joan Mannick study was merely a 6-week study whereas most rapamycin users are and will be taking them for years and years. And there were never any studies done on low weekly doses (with breaks) to conclude one way or the other.
Lastly, mTOR2 inhibition is dose-dependent? so 1mg daily x5 (vs 5mg one weekly) may not result in mTOR inhibition for the low-dose users as the blood serum level may not reach the inhibition level. Here I am just guessing though.
1 Like
I have no data, nor do you, on safety done daily long term - except in transplant patients, where we see lots of side effects. Sirolimus has a 62 hour half life, so whether you take it day or night time makes little difference - the serum level will be pretty similar after 5 half life’s of continuously taking a drug.
So we have data in long term cyclic use and a decent population doing this. Unless we have a population of healthy individuals doing this daily and collect data on actual outcomes rather than going back on forth on mechanisms and what one guesses might be the outcome - I’ll certainly not be heading down a continuous pathway until the safety profile is known.
I’d suggest we do not have a clear indication of safety in this situation unless there is data that has not been published or that I missed.
4 Likes
ng0rge
#68
May depend on your age, but for me at 70, sarcopenia is a real threat. I don’t want continuous, even low level inhibition of mTOR. I want plenty of time when mTOR is up, so I can build muscle. I’ll experiment with dosing but definitely plan on doing weekly to start and then maybe increasing the dose with longer breaks (10-14 days) in between.
1 Like
We worship the Mannick study because it’s the only human trial that we have.
1.FWIW the 0.5 mg daily dose had 35 total adverse events vs 46 TAE with 5 mg weekly.
2. In terms of efficacy it was close, but if you closely at the data the absolute change was more pronounced with daily dose.
3. Let’s remember also that total weekly dose of 0.5 mg daily dosing (3.5 mg) was lower than the once weekly dose of 5 mg.
So in summary what I see is slightly less TAEs and slightly better efficacy with over lower dose with daily rapamycin. One caveat there were more oral ulcerations with daily dosing.
I remain unconvinced that weekly dosing is superior to other more frequent dosing.
3 Likes
I’m not horribly interested in the Mannick study as that was a look at immune function. Does that correlate with leading to longevity, decreased cognitive decline? I don’t know. It was a short duration, so we know nothing of long term effects - which is much more what my worry is.
Dr. Alan Green on my search today doesn’t have complaints against him with the NY Medical Board. I’d say with 1500+ patients for many years, if he was having significant adverse outcomes, we’d likely see an investigation and complaints, because medical boards like addressing physicians with fringe or risky behavior - but need a complaint or adverse outcome. My gestalt is that he has integrity, and if he were seeing harm, he’d stop and also change his reporting of the use of rapamycin.
So he is going with cyclic - he has 400 patients for many years with hetero and homozygous APO E4’s without significant progression - again by his report. This is an outcome I have lots of patients interested in.
I have absolutely no idea if daily dosing is safe long term or effective. Until I have such data - which may well occur - I’d not want to start recommending this, then end up having harm occur, lack of efficacy etc. Especially harm.
It could be that daily is superior - but outcome data - at least the best we have, doesn’t favor either approach, because we only have the reports from Dr. Green on this, and I know this seems to be one safe approach. Is the other approach safe? I don’t know, but I’ve seen patients on daily sirolimus have serious problems - it wasn’t solely due that drug, obviously. But the side effects reported for daily use are above and beyond those expected even with the combination of drugs they are on …
7 Likes
AJD
#71
I think it’s rather clearly biased for Kaeberlein and others in this thread to jump to the conclusion that the Rapamycin dampened the allergic reaction.
I would suspect something quite different.
The Rapamycin may have undermined his immune response, leading both to the initial bacterial infection, and the hyper immuno-response causing the allergic reaction.
Maybe he would have had either no infection, or no reaction to an antibiotic were he not on Rapamycin.
We know, if only from the anecdotal reports of people in this community, that acne, which is an opportunistic bacterial infection, flares with the use of Rapamycin (in some people). I know that myself because I have experienced it. Why would it not also make us more vulnerable to other bacterial infections–and other abnormal immune responses?
Kaeberlein has, himself, made the case that Rapamycin “rebalances” the immune system. But, “rebalance” is a euphemism for “change”. It’s not at all clear that we have any idea how to predict exactly what those changes may be. Obviously, we all hope they will be net positive.
So, while I cannot argue that my scenario is necessarily MORE compelling than Kaeberlein’s assertion that the Rapamycin was likely a positive force in his antibiotic experience. I do think it is certainly at least AS LIKELY that it was the catalyst or amplifier for both the infection and the allergic reaction.
1 Like