adssx
#347
Several papers suggest that GLP-1RA might lower osteoarthritis pain besides weight loss, here’s the latest one (from India): Dual effects of dulaglutide on glycemic control and knee osteoarthritis pain in elderly patients with Type 2 diabetes
Elderly T2DM patients diagnosed with bilateral knee OA on conventional OA treatment for at least 3 months were studied for their glycemic metrics, OA pain scores and NSAID consumption at baseline, 3 months and 6 months.
Significant improvements in glycemic control were observed, HbA1c decreased from 8.7% to 6.5% over 6 months. Pain scores, NSAID, body weight and BMI showed substantial reductions over time. Positive correlation (r = 0.73, p < 0.001) was found between glycemic control and pain reduction.
Conclusion: Dulaglutide improves glycemic control, knee joint OA pain and weight management in elderly patients with T2DM.
The lower NSAID consumption is the most impressive results to me. TBC…
1 Like
adssx
#348
Comment in The Lancet: Muscle matters: the effects of medically induced weight loss on skeletal muscle
The importance of skeletal muscle mass is increasingly being recognised in the medical field. The crucial roles of skeletal muscle have come to the forefront of public attention due to data on the use of GLP-1 receptor agonists, which are effective for weight loss, but can cause substantial muscle loss. Studies suggest muscle loss with these medications (as indicated by decreases in fat-free mass [FFM]) ranges from 25% to 39% of the total weight lost over 36–72 weeks. This substantial muscle loss can be largely attributed to the magnitude of weight loss, rather than by an independent effect of GLP-1 receptor agonists, although this hypothesis must be tested. By comparison, non-pharmacological caloric restriction studies with smaller magnitudes of weight loss result in 10–30% FFM losses. In context, on an annual basis, the decline in muscle mass with GLP-1 receptor agonists is several times greater than what would be expected from age-related muscle loss (0·8% per year based on 8% muscle loss per decade from ages 40–70 years). Dismissing the importance of muscle loss can create a disconnect between patients’ increased awareness of muscle and the role it plays in health, and clinicians who downplay these concerns, affecting adherence to and the development of optimised treatment plans.
4 Likes
AglessRX now has oral semaglutide.
4 Likes
Apologies ahead of time, ignorant speculation follows, so if allergic to such, skip! I am pre-diabetic and intend to go on empagliflozin. I was considering GLP-1 agonists, but one big issue for me is that I do not need appetite suppression - this is not my problem, never has been. Basically, I have a set diet and I don’t deviate from it, plus I actually don’t get hungry. So all the stuff about how these drugs suppress appetite I don’t find a selling point.
Meanwhile, I wonder what other benefits do GLP-1 agonists have. Because the part where they increase insuling release are a negative as far as I’m concerned, as my pre-diabetes is not driven by low insulin (my insulin is on the high side already and I don’t need it to be higher!).
What I am interested in, are the unique advantages of the newer drugs over empagliflozin (and SGLT1/2i), for someone in my situation - I don’t need to curb cravings of any kind, I don’t need to lose weight, I don’t need psychiatric help/depression, sleep apnea, fatty liver, infertility and so on.
In that light, what do all these newer drugs do for me, compared to empagliflozin? I’m not saying they are worse by any means and I’m thrilled that they apparently help so many people, I’m just curious as to the bigger picture in a polypharmacy matrix, where someone is also taking other drugs such as pitavastatin and telmisartan - subbing terzapitide for empa gets me what? Again, apologies if I’m hopelessly unaware of some basic context.
DrFraser
#352
Not basic content and the GLP1’s IF you aren’t needing to lose some weight really won’t make a big difference in your HbA1C, maybe a bit in your insulin sensitivity. Now … for neurodegeneration, I like both GLPs and SGLT2’s.
If there is no weight to lose for example, on DEXA you are <20% fat and <1.8 lbs of visceral fat … taking a GLP could be harmful as you will lose some weight, and it is often preferentially muscle. However, if you are well above these figures, then a GLP could be a sensible item.
Most of my patients are on both a glp1 and sglt2 as they both have solid risk reduction to a whole bunch of the things that kill and disable people.
I don’t have a big concern about combining cyclic rapamycin, with these drugs and telmisartan. My reading of the literature would be a significant longevity benefit.
4 Likes
Thank you, DrFraser, and may I just add that I truly appreciate your contributions, it is nice to have someone here who has vast clinical experience. It is all well and good to pour over the literature on pubmed, as we all do, but actual practical real life clinical experience is invaluable and incomparable.
6 Likes
adssx
#354
What’s your eGFR? If below 90: empagliflozin or dapagliflozin make sense.
What’s your BP? Do you take telmisartan? (telmisartan can improve HOMA-IR)
Regarding your prediabetes and high insulin: what’s your HOMA-IR? As far as I know, SGLT2i do not lower sugar much (if at all) in non diabetic people. So it might not help you at all (although it can still be good for your kidneys, heart and brain). On the other hand tirzepatide (and maybe all GLP-1 agonists?) reduced the progression from prediabetes to diabetes by 92% in overweight people. Does this extend to people with normal BMI? No one knows. But no other class of drugs has ever gotten results as good.
Not everyone has appetite suppression with GLP-1RAs btw. And some like dulaglutide lead to mjnimal weight loss.
The issue with GLP-1RAs is that they increase insulin secretion. Although the results in the papers I found were not obvious. I’m testing oral semaglutide now and I’ll check whether it increases my fasting insulin or not.
3 Likes
Yes, my eGFR is above 90, HOMA-IR 3.3.
All my kidney numbers are very good (creatinine 0.82, BUN 12 etc.; urine test perfect). But my glucose control is clearly out of whack. My hope with empa is that dumping glucose can stabilize my numbers, and maybe even bring the A1c down from 5.9, and fasting glucose down from 113-117.
I just ordered the Abbott CGM, so I can see what is going on. Strangely, at least last year when I did a lot of finger blood strips, I rarely saw numbers above 140 post meals, so no crazy excursions, but bad morning glucose 110-115, and always elevated after exercise (110+).
With insulin at 12 uU/mL, I don’t want it to go up, so I’m afraid of GLP-1 agonists. Metformin at 500mg, over 8 months did absolutely nothing for me. I am slim, exercise quite a bit cardio and weights, good diet, no extra sugar, minimum saturated fat, tons of fiber, pescetarian-mediterranean etc. Very frustrating, which is why I am looking at pharma - I maxed out lifestyle.
My BP is elevated at 125-130 75-85, not on any BP meds, looking at telmi starting November.
1 Like
adssx
#356
The only way to know is to try. You should see quickly with empagliflozin whether it works or not. If not, you might want to try dulaglutide. 
2 Likes
Josh
#357
I might try that oral liquid from agless @DeStrider
Do you think its any different from Henry’s? People on reddit mostly seem tp say henrys doesnt work but they offer you to try the injection for just 50$ afterwards. Think agless would? Anything else to consider before i make a decision?
I believe that AglessRX is a good company and I would trust their products. However, I have not tried this one and cannot personally comment on it. But, if I were to buy one, I would consider it
Davin8r
#359
Ok but don’t say I didn’t warn you that it’s a complete waste of money. Sublingual absorption of these large peptides just doesn’t work. If it were that easy, Novo Nordisk or Eli Lilly would have just put their med in a sublingual tablet instead of (in the case of Rybelsus) using a special pharmacologic penetration enhancer that requires the pill to be taken on an empty stomach so that it gets absorbed across the stomach wall. My wife and I naively tried the HenryMeds oral tirz and it was worthless junk, although there was a small placebo effect at first. We switched to the injections and it was absolutely night and day difference.
2 Likes
adssx
#360
For it to work you need to keep it in your mouth for 5 minutes from what I remember. So quite impractical.
1 Like
Davin8r
#361
Even when taken at 3am and left to dissolve under my tongue x hours, it did nothing.
2 Likes
Josh
#362
Im going to try it from henry since theyll roll over the cost to injection if it doesnt work, and if it does work ill probably switch to agless.
1 Like
Davin8r
#363
Henry will NOT roll over the cost if you want to switch to injection. I tried that, and they wouldn’t do it.
3 Likes
Josh
#364
Huh, ive read stories on reddit of them doing it. Did you try within 30 days? I have read it has to be within 30 days of payment, not of receipt of product which is super lame, but workable if you know ahead of time as long as its not too delayed
Davin8r
#365
HenryMeds sends you the first TWO months of the pills but only charges you for the first month. If you take the refund of month one and then decide you want to do the injections, you have to first pay them for BOTH months before they’ll let you buy the injections.
Seriously, don’t waste your time and money on the orals. If you’re going to do a GLP, just do the injections. It is SO easy. Also, I’d consider lavenderskyhealth.com. They don’t even require a zoom call (just email “visit”), and they offer way more flexibility with how much you buy and which compounding pharmacy you want to use.
2 Likes
adssx
#366
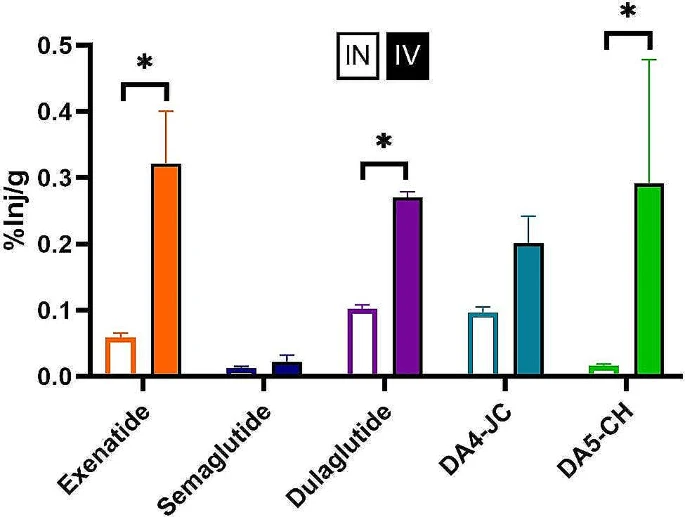
Another high-quality paper (Veterans Affairs) looked at brain uptake of GLP-1RAs, but this time via intranasal delivery: Comparing regional brain uptake of incretin receptor agonists after intranasal delivery in CD-1 mice and the APP/PS1 mouse model of Alzheimer’s disease 2024
Targeting brain insulin resistance (BIR) has become an attractive alternative to traditional therapeutic treatments for Alzheimer’s disease (AD). Incretin receptor agonists (IRAs), targeting either or both of the glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptors, have proven to reverse BIR and improve cognition in mouse models of AD. We previously showed that many, but not all, IRAs can cross the blood-brain barrier (BBB) after intravenous (IV) delivery. Here we determined if widespread brain uptake of IRAs could be achieved by circumventing the BBB using intranasal (IN) delivery, which has the added advantage of minimizing adverse gastrointestinal effects of systemically delivered IRAs. Of the 5 radiolabeled IRAs tested (exenatide, dulaglutide, semaglutide, DA4-JC, and DA5-CH) in CD-1 mice, exenatide, dulaglutide, and DA4-JC were successfully distributed throughout the brain following IN delivery. We observed significant sex differences in uptake for DA4-JC. Dulaglutide and DA4-JC exhibited high uptake by the hippocampus and multiple neocortical areas. We further tested and found the presence of AD-associated Aβ pathology minimally affected uptake of dulaglutide and DA4-JC. Of the 5 tested IRAs, dulaglutide and DA4-JC are best capable of accessing brain regions most vulnerable in AD (neocortex and hippocampus) after IN administration. Future studies will need to be performed to determine if IN IRA delivery can reduce BIR in AD or animal models of that disorder.
So, intranasal semaglutide still doesn’t cross the BBB and is worse than IV exenatide. Intranasal exenatide and dulaglutide are quite impressive! How easy is it to do IN if you buy the normal drug? And how do you scale the dose? 
(DA4-JC and DA5-CH are dual GLP-1/GIP receptor agonists so they might be even better. I don’t know if they’re commercially available or in an R&D pipeline. Any idea @Steve_Combi?)
With dulaglutide, uptake in females is a bit lower, and the authors note that “Since brain uptake following IN delivery of dulaglutide and DA4-JC is not saturable, it may be possible to compensate for sex-related decreases in uptake in some brain regions of AD cases by increasing the IN dose.”:
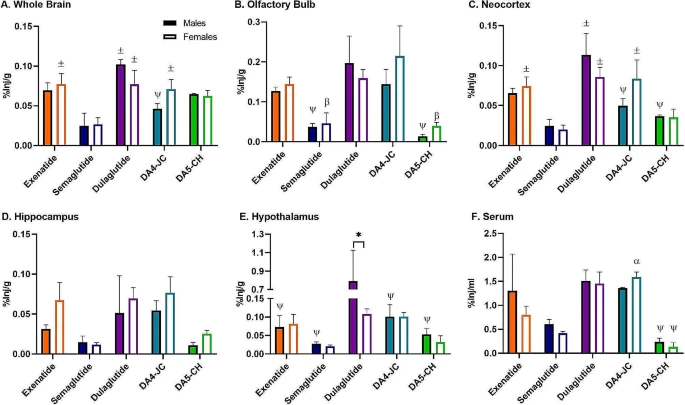
A growing body of evidence in favor of dulaglutide in non-overweight people @DrFraser?
If liraglutide (that does not cross the BBB) can slow down cognitive decline by 18% (see: Intermittent (oral) Rybelsus / Semaglutide use in healthy individuals? - #291 by AnUser and the paper: Evaluation of Novel GLP-1 analogue in the treatment of Alzheimer’s disease 2024), then, what could dulaglutide do?! And how come there is no trial of dulaglutide for MCI, AD, or PD? I assume that people are waiting for the results of the phase 3 exenatide trial in PD (due to be published in a few months) before launching a new one.
6 Likes