I don’t think these peptides should be dosed on a multi-day per week basis. They have a long half life of 6 days so you have the opportunity to have a higher level of GLP1=R’s that one thinks. And the level would stay constant at a point in time with no decline and no peak.
The studies in 10’s of thousands of people, indicate what works.
Weekly dosing allows a high peak and a decline that I believe is beneficial. I see a lot of people on social media complain about plateaus, no effects, “desensitization:” etc who are following influencers who promote this multi-day per week thing.
My experience with more than a few clients is that sticking to the prescribed method of once weekly of an effective dose works. I’ve not had anyone complain when following the protocol the peptide was designed for. It was not designed for multiple doses per week.
2 Likes
LukeMV
#185
I am not saying I disagree with you, but I think another reason it is primarily done is to avoid side effects the same way some people inject testosterone daily instead of 1-2x per week. I’m trying to be a bit cautious of bolus dosing since I’ve heard enough people say too high of a dose made them sick so I think this is a good way to assess my tolerance. I might go to less frequent dosing later on.
1 Like
There isn’t a downside that I can think of to daily dosing at 1/7th the weekly dose, apart from filling landfills with syringes, and jabbing oneself more frequently.
I think @Steve_Combi has a valid point, with T1/2 of 6-8 days depending on agent for SG/TZ/RT there isn’t a clear reason to have split dosing. I guess if someone had intolerance, after changing agents, I might split it twice weekly - but ultimately, the efficacy of the agent is hand in hand with it’s toxicity. So if you don’t tolerate the toxicity, you won’t get the benefits.
For me, I have not a single side effect when I take a GLP … so I only get the benefit. I’ve got patients who on 0.25 mg/week of semaglutide are very unwell. They obviously are not going to be a candidate for this being part of their weightloss success.
4 Likes
LukeMV
#187
Ok I am on day 7 and I am definitely getting a faster heart rate and appetite control (not suppression) now. I definitely will not be raising the dose. I will either stick to 0.5mg daily or go back to this dose every other day.
2 Likes
Rob01
#188
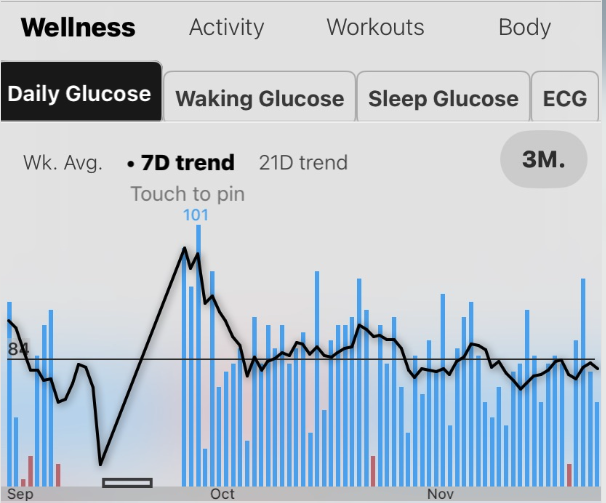
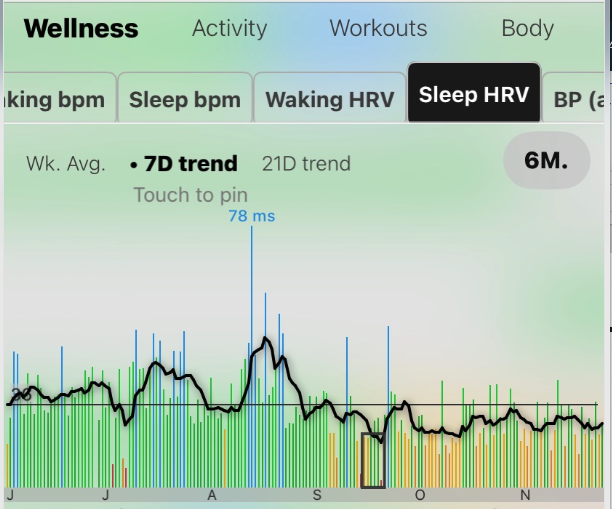
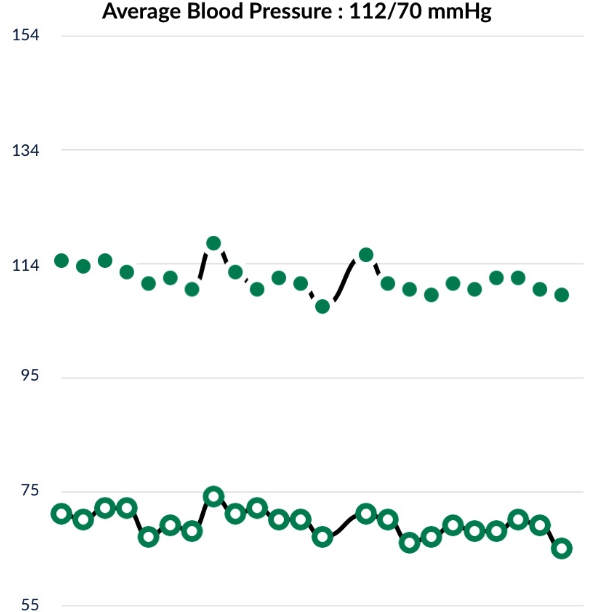
Some stats from my use of TZ (1mg escalating to 4mg over 3 months). I started TZ in mid Sept this year. About to turn 50 in a couple months. When I initiated this experiment I was already in pretty good shape and vitals were pretty good. So this was an optimization. I also had the hope to stop/reduce snacking which can be more or less depending on what’s around the house.
My abreviated anaylsis is that:
- Sleep HR initially rose but came back down
- Sleep HRV took a hit and has not recovered yet. Being patient on that.
- Fasting Glucose (reads in the pic as Daily Glucose) has been reducing per goal. I tried Metformin for 3 months before the GLP as well for contrast.
- Blood Pressure is also lowering
I’ve listed my goals in an earlier post here (Longevity and many factors associated with longevity) and I measure progress based on FG, BP, and hsCRP as general proxies for overall health improvement. I’ll get my 3 month hsCRP in the next couple weeks to see if that’s improved. Note weight is not a goal for now. I started at 150 and eat to maintain 150 lbs. I’m adjusting (increasing) dose based on the easily measurable targets.
- FG in the low 80’s
- BP 110 / 68
- hsCRP < 0.5
Also included is a pic from the weekend in the morning. I wish I took a before pic 

8 Likes
Isn’t it the greatest feeling? Every time I walk by a mirror now that I am pretty much at goal, I think - is that me? Is that my body? Going from XXL clothing to Medium in the 18 months I’ve been on the GLP1 journey has been so life changing. Having been heavy since my early teens (over 50 years ago), the change has been so gratifying and the taking away of the “food noise” helped make this possible.
13 Likes
Thanks for all you have done in educating folks in the world of peptides, Peppys started me down the path of self learning in the area of longevity.
1 Like
LukeMV
#191
How long did it take for your heart rate to go back down? Mine is bad enough from just beginning retatrutide that I have had to take extra Nebivolol to lower it.
1 Like
Davin8r
#192
Do you find nebivolol helps? Raising the dose of nebivolol didn’t make a difference for me, and the rodent study that showed a direct effect on the SA node of the heart also found no effect of beta blockers and speculated that a calcium channel blocker would be needed.
2 Likes
LukeMV
#193
I’m glad I mentioned that because so far, it hasn’t lowered my heart rate any more at all either. So a CCB might lower it instead? I wish I had one handy. I had trouble falling asleep last night because my heart was racing so much.
Davin8r
#194
In theory, but only a calcium channel blocker that has chronotropic (heart rate lowering) effects like verapimil or diltiazem. Maybe your PCP would work with you on this(?)
2 Likes
I’m glad to be able to be able to help others.
1 Like
LukeMV
#196
Actually I completely forgot but I ordered some
verapamil a long time ago that I never used. Maybe it’s time to finally try it out. I just have to figure out if it’s safe to use with 5mg Nebivolol as I’d prefer not to stop taking that. I’m also taking 40mg Telmisartan.
I could start with 40mg verapamil and go from there
DrFraser
#197
Verapamil is a bit of a bad player for causing bradycardia, especially when used with a beta blocker.
With caution, I’ll use diltiazem + a beta blocker, but not in elderly patients … I’ve seen so many cases of symptomatic bradycardia, heart block with this combination, which gets much more common with advanced age.
3 Likes
LukeMV
#198
What about for someone who isn’t elderly, owns a blood pressure monitor, and carefully wants to lower a resting heart rate of 80 from a GLP1?
Rob01
#199
It took 2-3 weeks for my heart rate to normalize again once I started Trizepitide though I never had issues like a racing feeling or difficulty to go to sleep. You might think about a lower the dose a bit until everything stabilizes then slowly up the dose. For me I started at 1 mg TZ / week for 2 weeks until everything felt normal then increased the dose to 1.5 mg for 2 weeks until everything felt normal and then continued that pattern up to 2 mg twice a week for a total of 4 mg / week. When I started at 1 mg the hunger suppression to aversion, fatigue and bloating were unpleasant but after ~ 2 weeks my digestion returned to normal, the fatigue was gone and hunger was just suppressed a level. I remember one morning in the first 2 weeks where I was sitting at the kitchen table to get my shoes on to go to the gym and I was thinking I’m too fatigued to put on my shoes much less drive to the gym and then workout. I still did but had to drag myself.
3 Likes
DrFraser
#200
Sure, it’s fine, I’d recommend, in general, use of diltiazem with a beta blocker (instead of verapamil). I also have more comfort, due to clinical experience with bisoprolol, metoprolol or carvedilol in this situation.
1 Like
LukeMV
#201
Have you seen Diltiazem or Verapamil impair training performance at the gym at low dosages like beta blockers typically would (except Nebivolol)?
My clinical experience is verapamil is a much worse agent … but I put it out to AI … and it agrees:
Verapamil and diltiazem are both calcium channel blockers (CCBs) used to manage cardiovascular conditions such as angina, hypertension, and atrial fibrillation. Their impact on exercise tolerance varies due to differences in their pharmacological effects.
Verapamil is known for its more potent negative chronotropic and inotropic effects, meaning it can significantly reduce heart rate and myocardial contractility. This can lead to reduced exercise tolerance, as the heart’s ability to increase output during physical activity is limited. Patients may experience fatigue and weakness during exercise, and maximal exercise capacity might be restricted 1.
Diltiazem, on the other hand, has moderate negative chronotropic and inotropic effects, which generally result in better exercise tolerance compared to verapamil. It allows for a more balanced heart rate and contractility during exercise, making it more suitable for patients who engage in physical activity. Studies have shown that diltiazem can improve exercise tolerance in patients with chronic stable angina by increasing exercise duration and delaying the onset of angina 1.
In patients with chronic atrial fibrillation, both verapamil and diltiazem can modestly improve exercise tolerance by reducing ventricular rate, although the improvement is similar between the two drugs 1. For angina pectoris, both drugs increase exercise capacity by delaying ischemia onset, with no significant differences in maximum effort parameters 1.
In conclusion, while both verapamil and diltiazem can improve exercise tolerance in certain cardiovascular conditions, diltiazem is generally better tolerated during exercise due to its moderate effects on heart rate and contractility. The choice between these medications should consider the specific cardiovascular condition, patient characteristics, and potential side effects, with diltiazem often offering a better safety margin for those who are physically active.
3 Likes
LukeMV
#203
Thank you. Sounds like Verapamil would be a terrible choice for me. I’ll just ride out the heart rate for now and hope it normalizes.
2 Likes