A_User
#22
Wouldn’t an Aktiia monitor be good in your case as well?
Since you’ve already blacked out once maybe it’s important to be careful and not lower it too much, or it might be something else as well.
2 Likes
Thank you for your advice. I have ordered the Contec device you recommended. @DrFraser
1 Like
I just got my Contec BP monitor. It’s saying my SBP is around 116-123/76 while I’ve been using Telmisartan 20 mg daily. That doesn’t sound too bad to me. Surely nothing that would cause me to blackout. It must have been tied to the nausea.
Nausea commonly causes a vasovagal reaction, which can drop blood pressure and heart rate.
I obviously didn’t assess you - but we see this frequently in the ER - actually treated one of these yesterday.
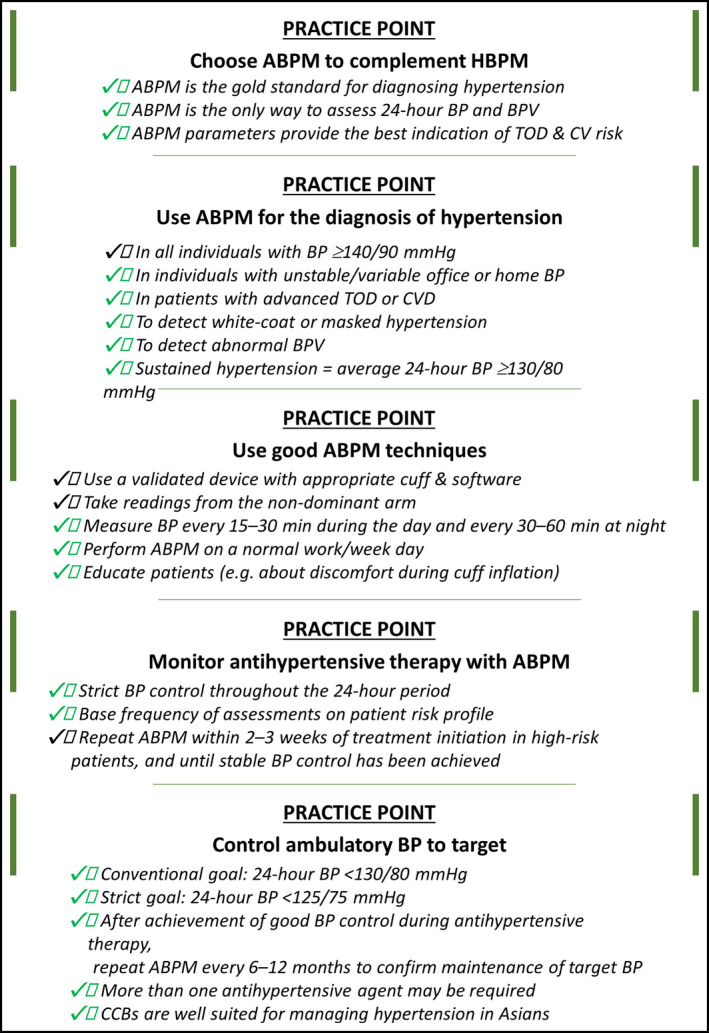
The good thing is you can also look at your BP variability and whether it has a normal pattern overnight, etc. I think doing a 24 hour ambulatory if on BP meds (or not) is sensible quarterly.
1 Like
A_User
#26
BP is usually higher during the day (or periods of wakefulness) and lower at night (or periods of sleep). The expected physiological fall in nighttime BP is > 10% (dipping), whereas a reduction of < 10% in BP at night is defined as non‐dipping; patients with a riser (or reverse dipping) pattern show an increase in BP during sleeping hours to levels (BP fall is < 0%) that may be higher than those during the day (ie, nocturnal hypertension). 34 Extreme dipping refers to patients who show a marked (>20%) nocturnal fall in systolic BP (SBP) and or diastolic BP (DBP), or have a night/day SBP or DBP ratio of < 0.8. 20 Given that the circadian rhythm of BP is predominantly determined not by awake‐sleep behavior rather than the day‐night cycle, 35 the nocturnal dipping status of shift workers should be determined by awake BP (during nighttime) and sleep BP (during daytime).
Nocturnal BP may be the most reproducible and reliable ABPM parameter for risk stratification. 36 Nocturnal hypertension (BP ≥ 120/70 mmHg) could indicate the presence of comorbidities such as obstructive sleep apnea (OSA), and the riser pattern of nighttime BP is associated with a particularly poor prognosis with respect to the occurrence of stroke and cardiac events. 37 , 38 , 39 Stroke risk also appears to be increased in elderly hypertensive patients with an extreme dipper pattern. 40 Another important BPV parameter is the morning BP surge (the difference between the lowest nighttime BP and morning BP measured 2 hours after awakening). Early morning BP surge is associated with an increased risk of cardiovascular and cerebrovascular adverse events, especially hemorrhagic stroke. 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52
Excessive BPV could result in large dynamic surges that have the potential to trigger adverse cardiovascular events (the resonance hypothesis), and the risk of these events is exaggerated in high‐risk patients with vascular disease. 53 Greater variability in SBP is a significant independent predictor of mortality. 54 , 55
Aktiia (Hilo) isn’t useful for this right now because it’s inaccurate at night.
2 Likes